Q & A Billing
Quick Answers to Your Questions!
Generate Claim
- I clicked the "Get it Ready for Billing" button, but my claim is not in the "Generate Bill" tab. Where did it go?
-
[Minnesota] Why is my T1019 UA in the "Not Billable" tab due to a missing UMPI number?
Claim Detail Report
- I voided a claim, but I cannot delete the timesheet. Why?
- What is a payer control number? I see an error that I have to enter this when trying to void a claim.
- Why is my claim denied?
- Fixing a Claim
- Why was my waiver was sent with the employee UMPI?
- My claim has the "Sent Status Request to Payer," what does this mean?
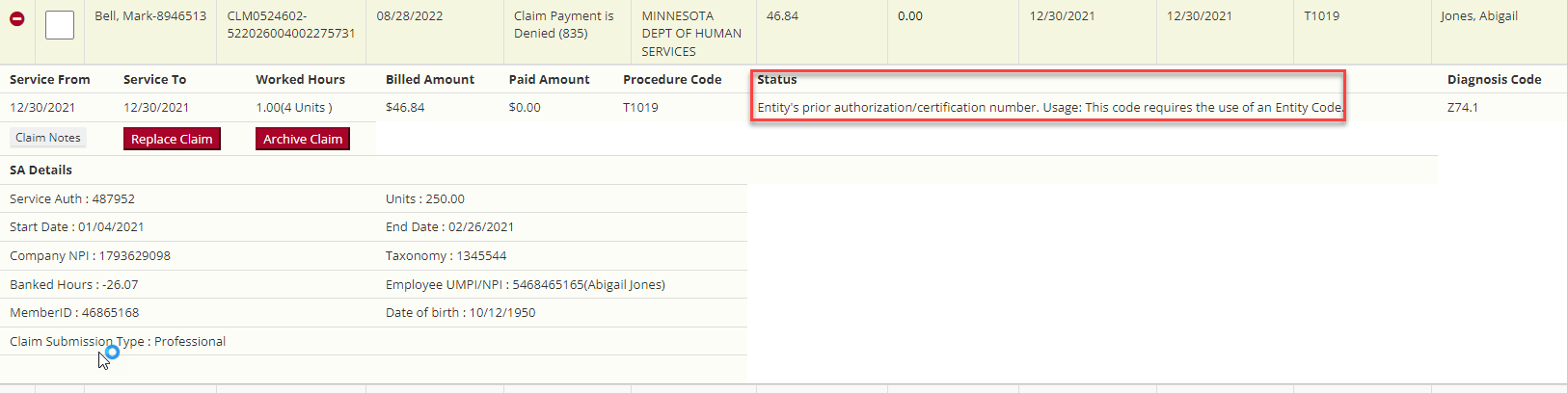
- What is an Entity Code?
- What is a remark code?
I clicked the "Get it Ready for Billing" button, but my claim is not in the "Generate Bill" tab. Where did it go?
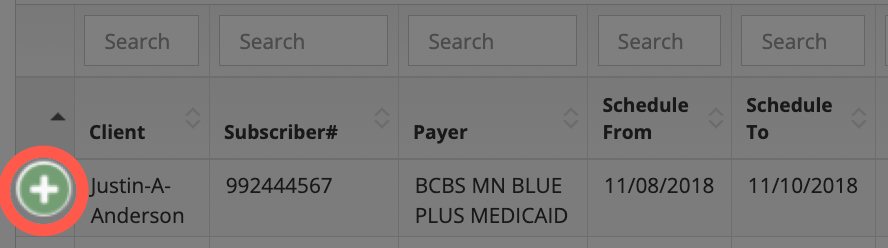
Check the “Not Billable” tab. If the claim appears here, click on the + sign to the left of the client’s name to check the “Missing Details”.
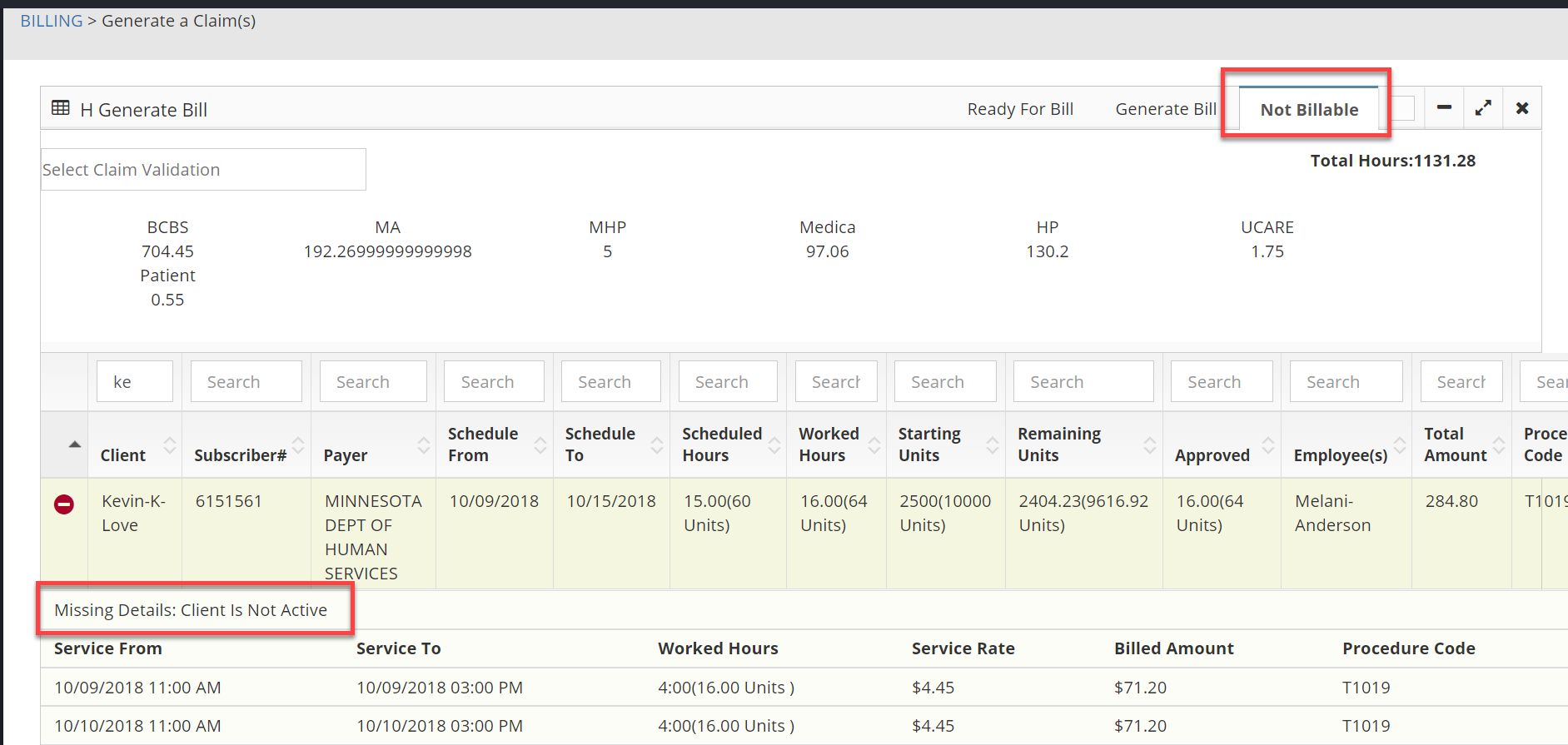
Once the missing details have been corrected, the claim should automatically move to the “Generate Bill” tab so it can then be billed.
Why is a claim showing in the "Not Billable" tab?
This question can be answered by clicking on the + sign to the left of the claim line within the "Not Billable" tab.
Upon doing so, a section for "Missing Details" will be displayed.
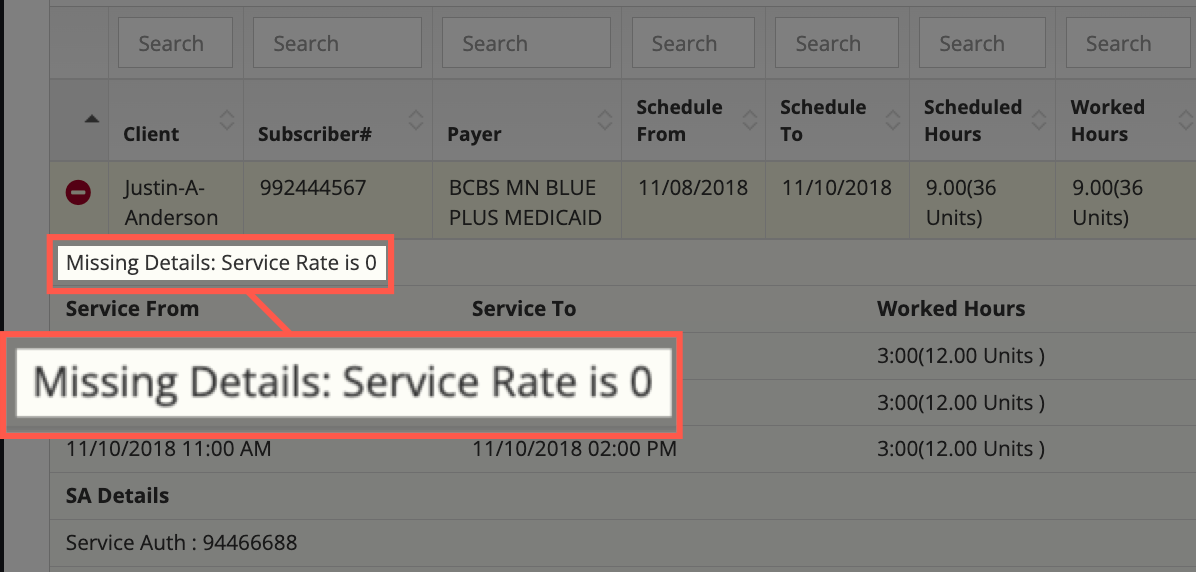
Here are a few examples of reasons that a claim could be in the "Not Billable" tab:
- Service Rate is 0: This means that a service rate was not input into the service authorization that was entered into the system. To correct this, locate the service authorization and update the service rate field.
- Client is not active: In order to bill a claim, the client must be in the "Active" status.
- Employee UMPI: In the service authorization, the "Wavier" checkbox was not checked so the system is looking to make sure the employee's UMPI number was input. In this case, it was not. To correct, the employee's UMPI number would need to be added into their employee profile (or the "Wavier" box would need to be checked in the service authorization if employee UMPI number is not needed for the claim).
- Patient out of hours: The number of hours being submitted exceeds what is allowed by the service authorization that was entered into Billiyo.
Once the "Missing Details" have been corrected, the claim should automatically move to the "Generate Bill" tab so that it can be billed.
[Minnesota] Why is my T1019 UA in the "Not Billable" tab due to a missing UMPI number?
If your employee is working a T1019 UA, enter your agency's PCA NPI as their UMPI number in the employee's profile.
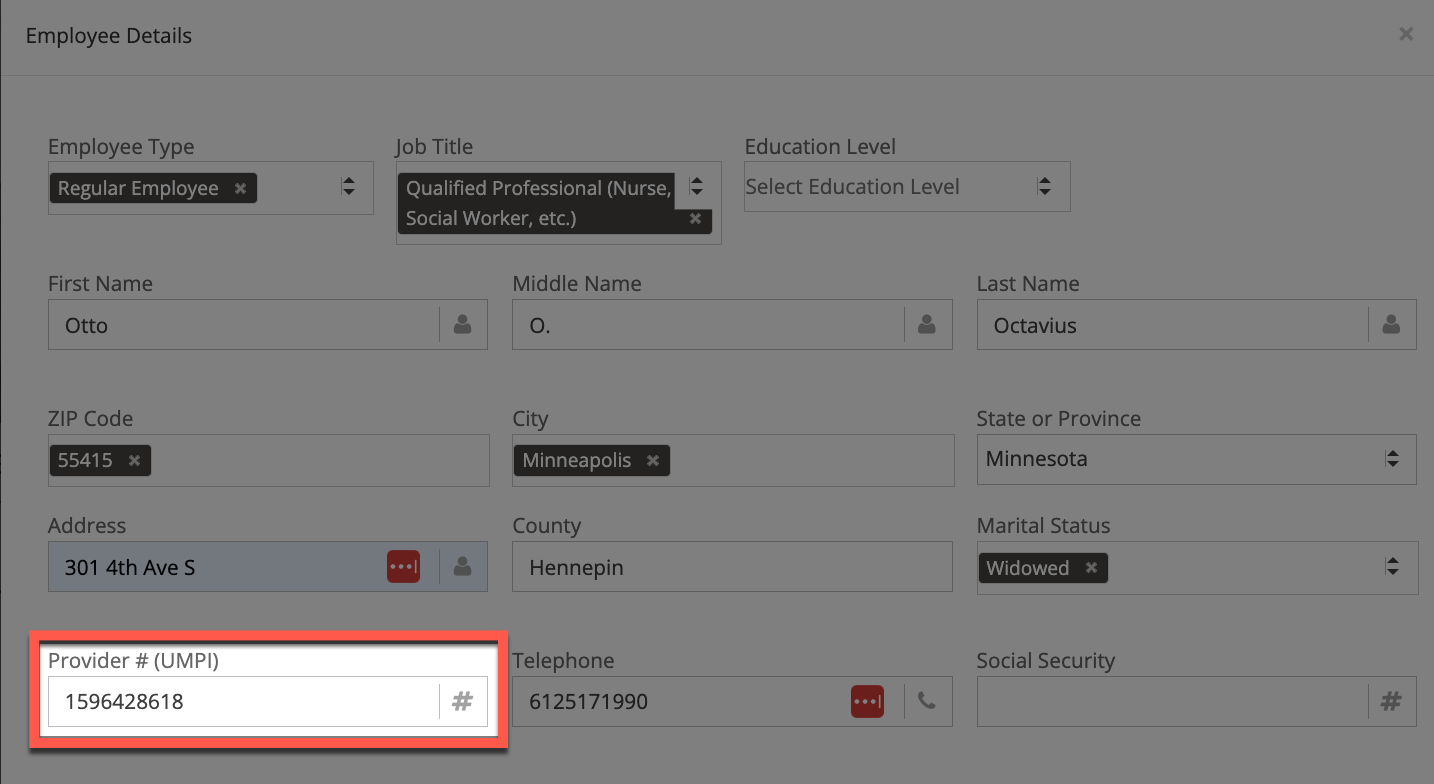
Alternatively, we can check the "Wavier" checkbox in the service authorization as this will alert the Billiyo system to send the agency NPI/UMPI instead of checking for an employee UMPI number.
I voided a claim, but I cannot delete the timesheet. Why?
There is likely another claim that has been billed for this timesheet.
Every claim that is generated needs to be voided before the timesheet can be deleted. If a timesheet covers two months, then it will be split into two claims — one claim for each month.
What is a payer claim number? I see an error that I have to enter this when trying to void a claim.
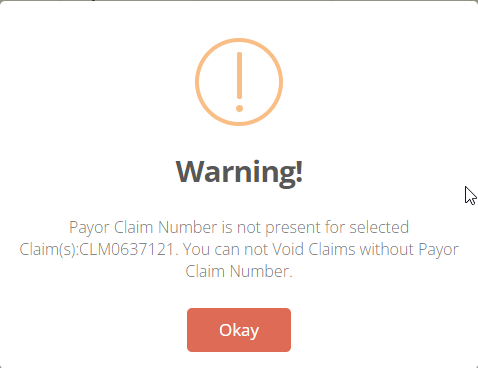
The “Payer Claim Number” (Payer Control Number) is the number that is assigned by the payer to identify a claim and can be found within the payer’s system. The “Payer Claim Number” (Payer Control Number) has to be present in order to void a claim.
To resolve the above error message first pull the “Payer Claim Number” (Payer Control Number) from the payer's system. Then go back to the claim detail report, expand the claim, and click the "Claim Notes."
If you need any help locating your payer claim number, please contact the payer.
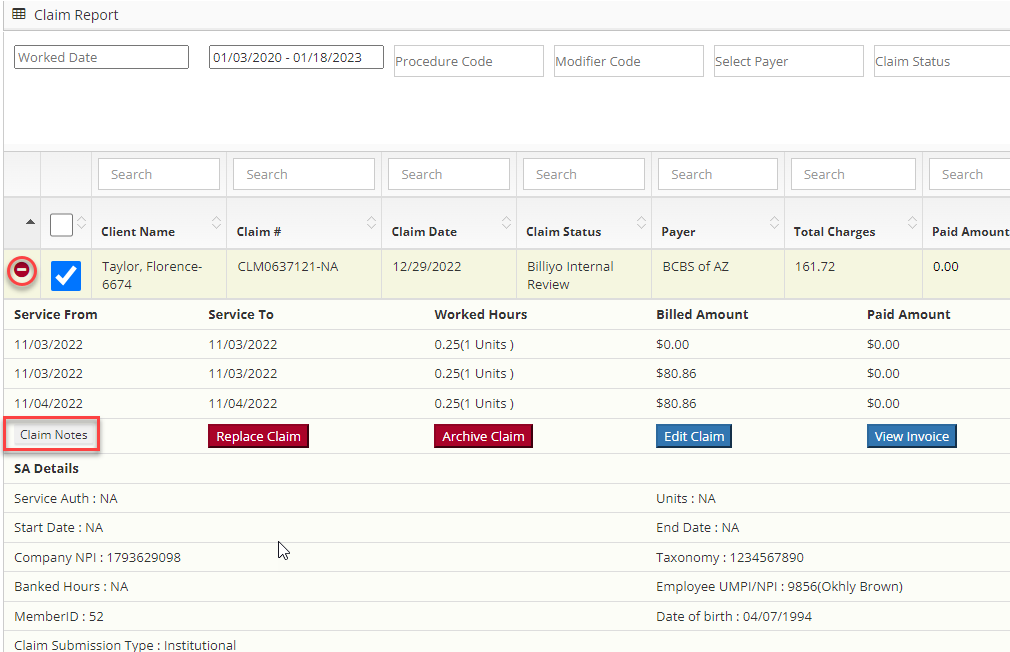
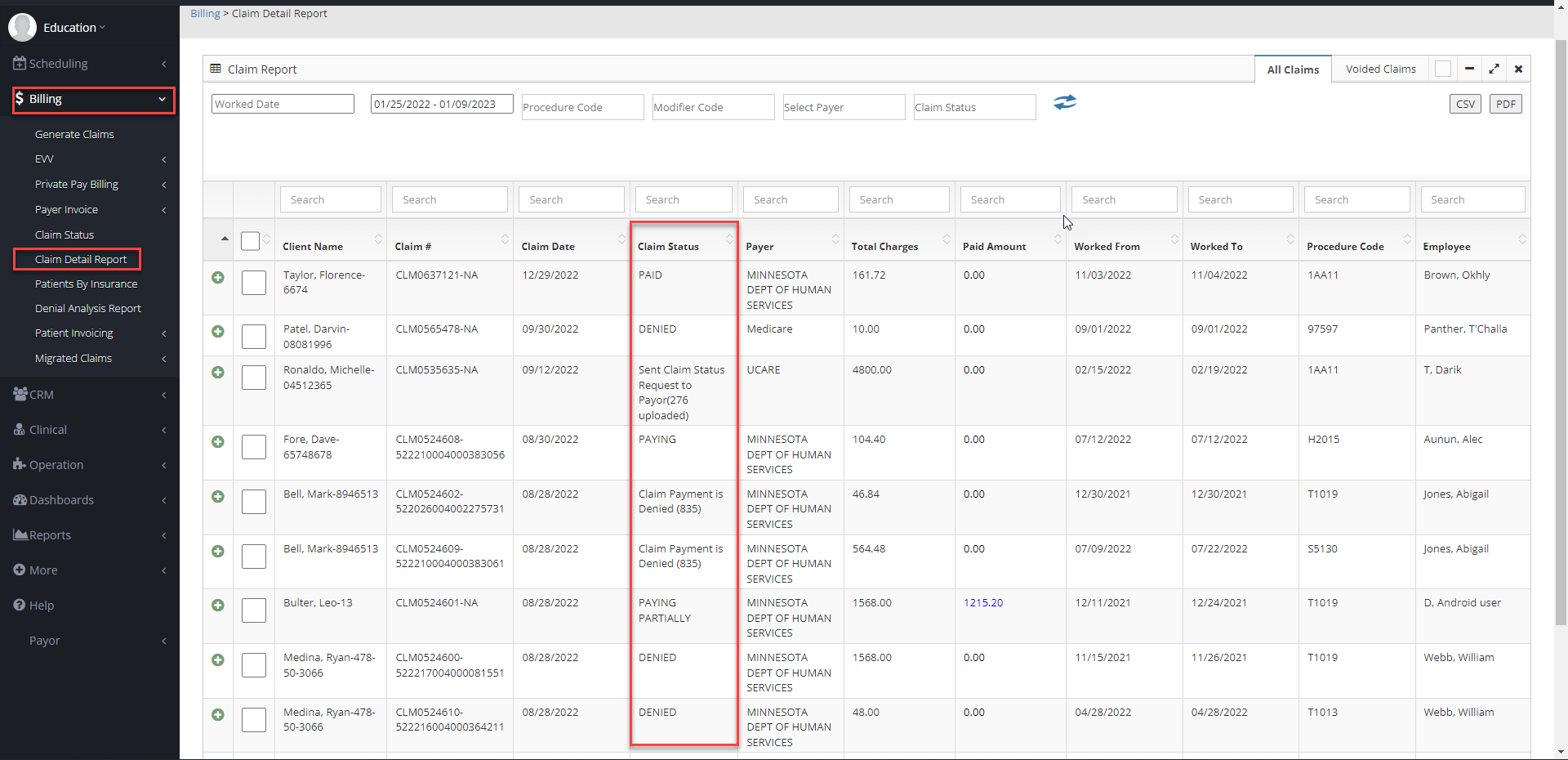
In the resulting pop-up click on the pencil icon and enter the “Payer Claim Number” (Payer Control Number).
Finally, click on the check mark to save this information. After, the claim should be able to be voided.
Why is my claim denied?
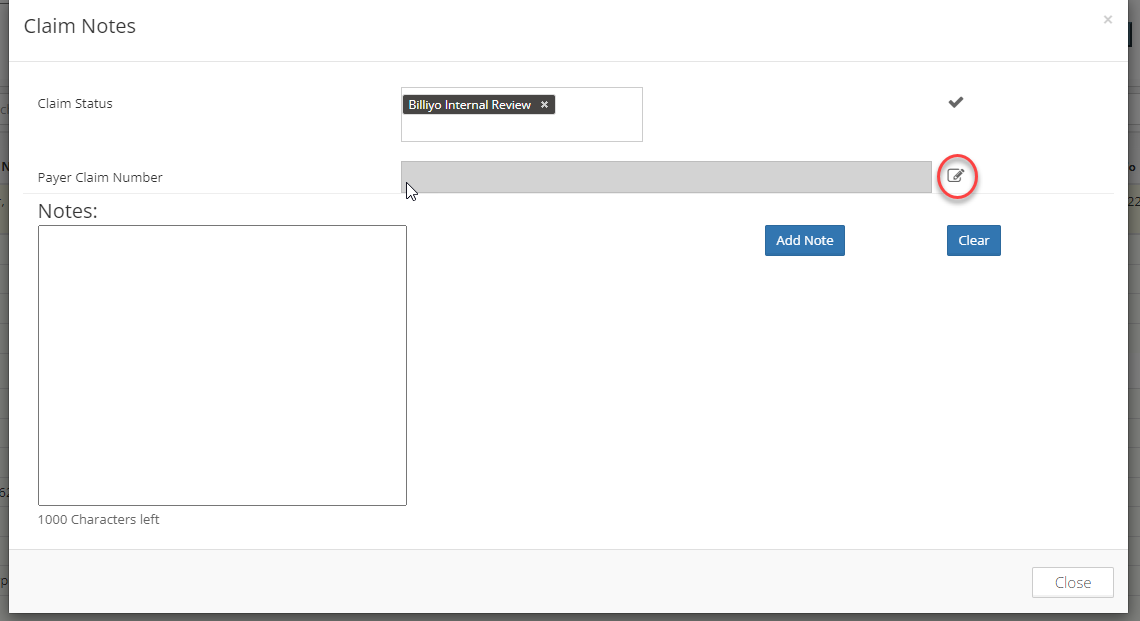
Claims could be denied for multiple reasons. Learn which claims are denied by navigating to Billing > Claim Detail Report.
Locate the claim and check it's status. Here we can see whether or not it was paid, denied or partially paid.
To view a claim in more detail, click on the + sign to the left of the client’s name and in this expanded menu there may be a “status” field that may contain additional information.
To learn more about denied claims go to the Claim Denial Analysis Report (Billing > Denial Analysis Report). Search for the claim and click on the + sign by the employee's name. In the denial category an explanation as to why the claim was denied should appear.
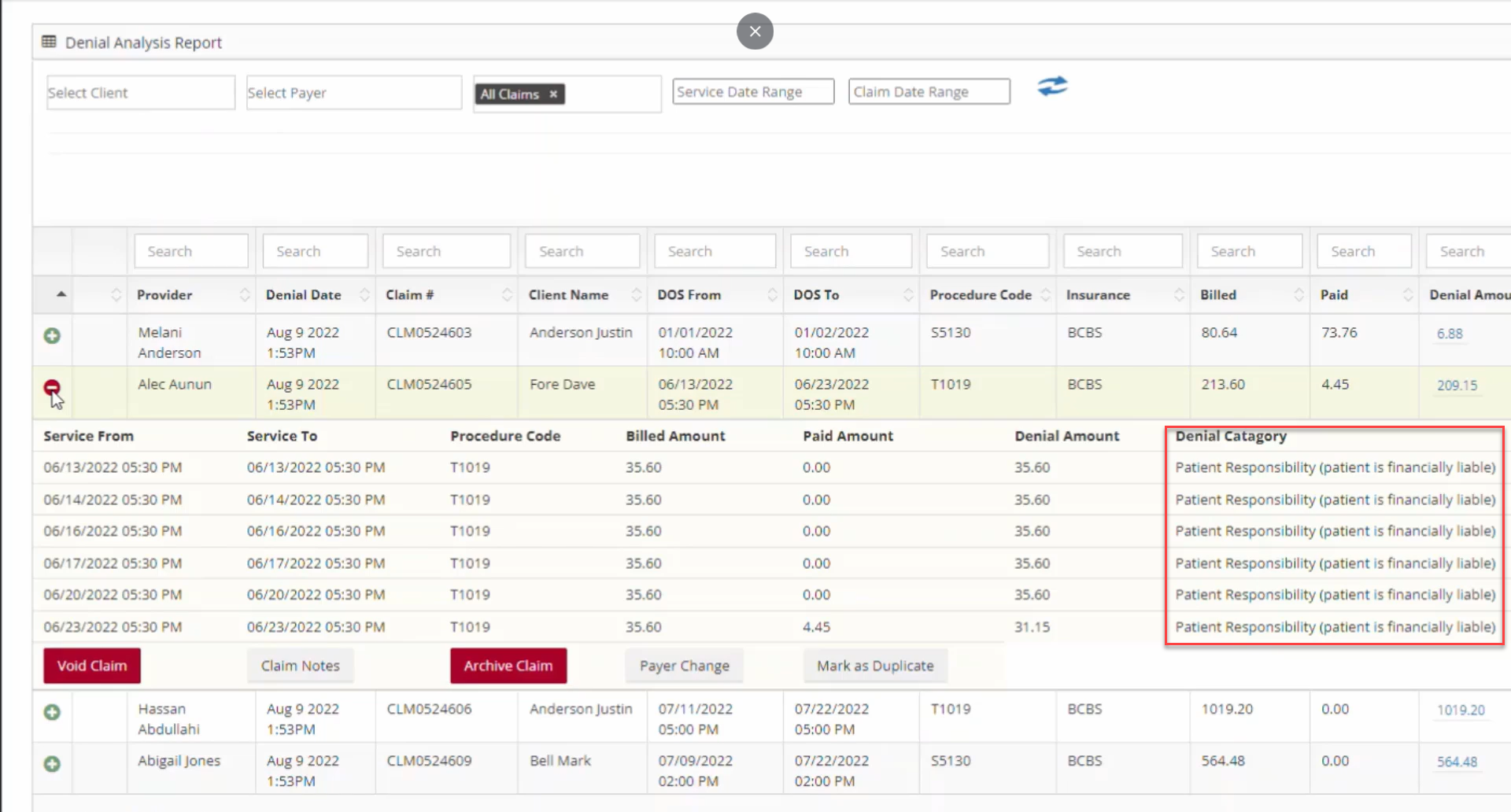
If you need further clarification, please reach out to the payer for more information. Remember, the claim number you see in Billiyo should match the claim number in your payer's system.
Process of Fixing a Claim
Learn more about why a claim was denied by using our Denial Analysis Report, or contacting the payer directly. Once the reason for denial is known, head back into Billiyo to make adjustments.
Here's a quick example. If a claim was denied because it was not marked as a waiver service in the service authorization, and it should have been, go to the service authorization and check the "Waiver" checkbox.
If a claim was denied because of a mistake in the visit itself, it will need to be voided (in the Claim Detail Report page). The schedules will appear again in the Schedules Approval page where edits can be made to them.
After fixing the incorrect information, head back to the Claim Detail Report page to take action. Locate the claim and click on the checkbox to the left of it to see the following actions: rebill, replace, void.
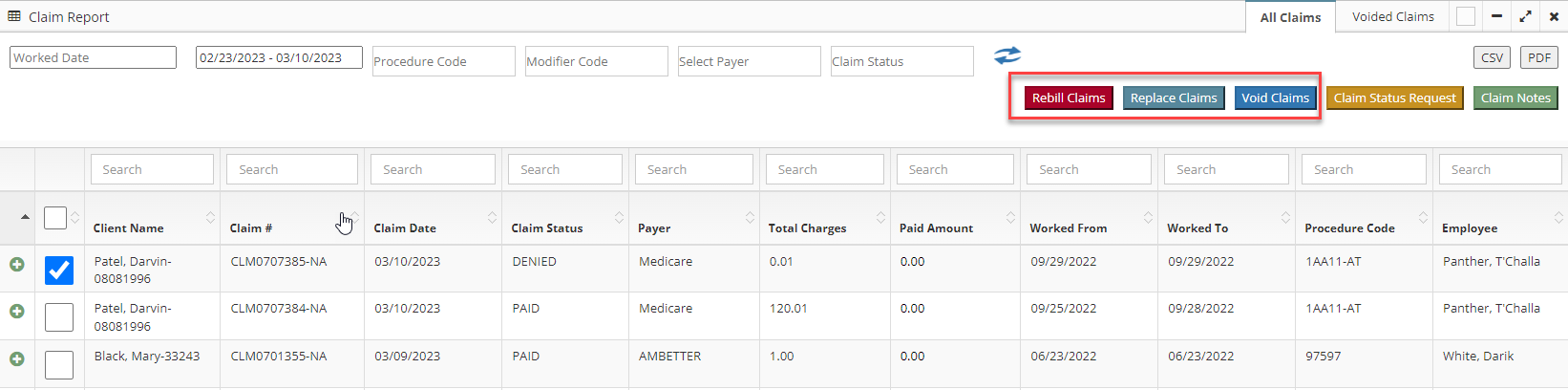
Click Here for a detailed walk through of fixing denied claims.
Why was my waiver was sent with the employee UMPI?

If you see that your employee's UMPI was sent with a waiver service, this is because the service agreement that this claim was made for was not set as a waiver. To resolve this, head over to the service auth [CRM > Service Auths > Add/View SA]. that that this claim was made for.
You can see the service auth number in the claim detail report.
After locating the agreement, hit its green plus sign and then click on the blue pencil icon.

This will create a pop-up where we can edit the agreement. In the edit service authorization page there will be a waiver check box.

When this checkbox is disabled, your employee's UMPI number is sent with the claim. When this waiver box is enabled, the company NPI is sent instead.
My claim has the "Sent Status Request to Payer," what does this mean?
The "Sent Status Request to Payer" status means that Billiyo sent a status request to your payer. This occurs after the payer/clearing house accepts your claim.
If we are receiving your ERA, the payer may provide Billiyo with an update concerning the claim before they officially pay or deny it.
There is no guarantee that the payer will provide a status update. If they provide one to Billiyo we will display it the claim detail report and denial analysis report.
If we are not receiving your ERA, then we will not get a status update until the claim is paid or denied.
If a claim has the Sent Status Request to Payer status for more then a week, then your claim was most likely denied. In that case, reach out to your payer and ask them for a update on the claim.
What is an Entity Code?
"Entity's prior authorization/certification number. Usage: This code requires the use of an Entity Code." is a generic denial reason and it could mean a multitude of things. Billiyo receives this text directly from your payer but we do not get any further clarification.
When you see this error, first check your service agreement and make sure that its correct. If it is, you will need to consult the Denial Analysis Report or call your payer.
If you do not know why a claim was denied, your Billiyo CSM will not be able to tell you. Please reach out to your payer, they denied your claim and they will know why.
What is a "remark code"?
"Claim/Service denied. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) is a generic denial reason and it could mean a multitude of things. Billiyo receives this text directly from your payer but we do not get any further clarification.
When you see this error first check that your service authorization is correct. If it is, you will need to call your payer and ask for clarification on this claim
If you do not know why a claim was denied, your Billiyo CSM will not be able to tell you. Please reach out to your payer, they denied your claim and they will know why.