Denial Analysis Report
The Denial Analysis report lists all claims that are denied by payers and the reason why they were denied.
Jump To:
Viewing
Updating
Downloading
Viewing
To view the denial analysis report, head to "Billing" > "Denial Analysis Report". .gif?width=688&name=2022-07-11_15-31-40%20(1).gif)
On the screen that appears, use the filters at the top to help locate a specific claim — make sure to click on the blue arrows to refresh the results. The search fields above each table heading can also be used for further refine the results.

Denied claims will be selected by default in the "Select Report Type" field. This can be changed to filter for partial payments, duplicate claims, or all [denied] claims.
Click on ![]() to the left of the "Provider" to view the details of the claim. Additional information as to why a claim was denied or partially paid should show here.
to the left of the "Provider" to view the details of the claim. Additional information as to why a claim was denied or partially paid should show here. 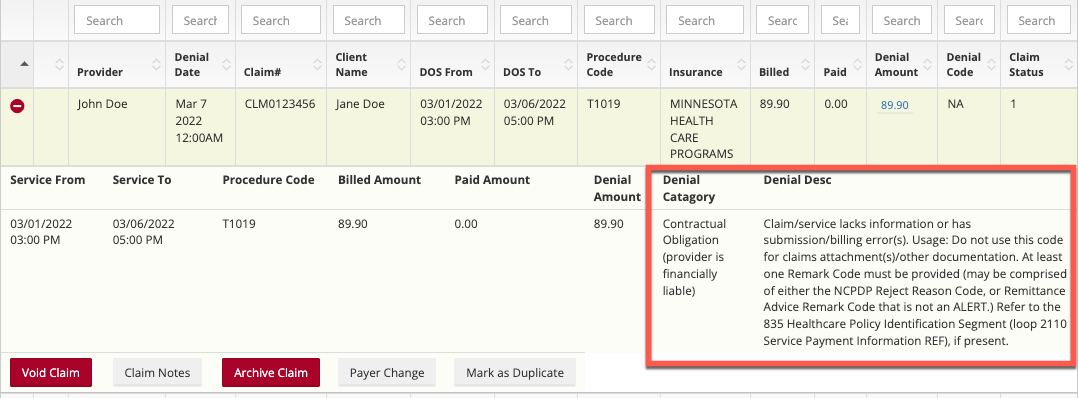
Updating
After clicking on the ![]() to the left of a claim buttons to void the claim, add notes, archive, mark payer change and mark as a duplicate will appear.
to the left of a claim buttons to void the claim, add notes, archive, mark payer change and mark as a duplicate will appear.
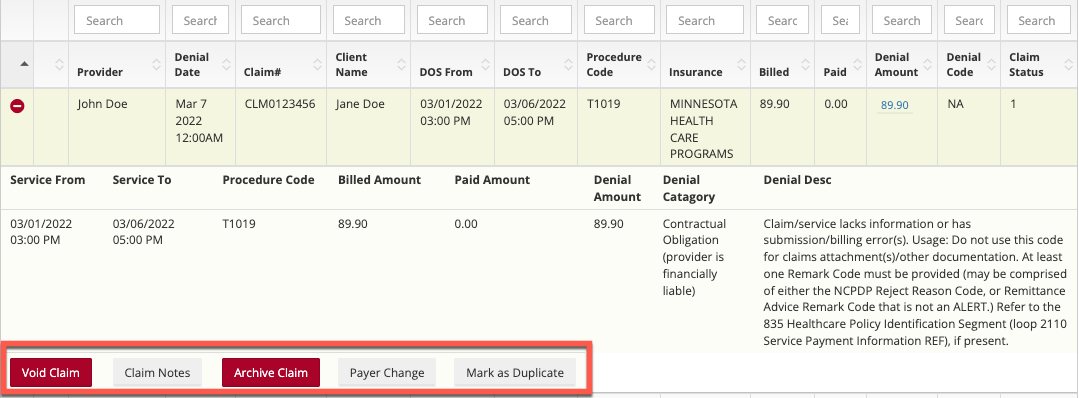
After voiding a claim, and fixing the issue, you can rebill the claim — generating a new claim.
Claim Adjustment:
The amount amount of money that you claimed is indicated by the Billed tab and the Amount that the payer paid is shown in the paid tab.
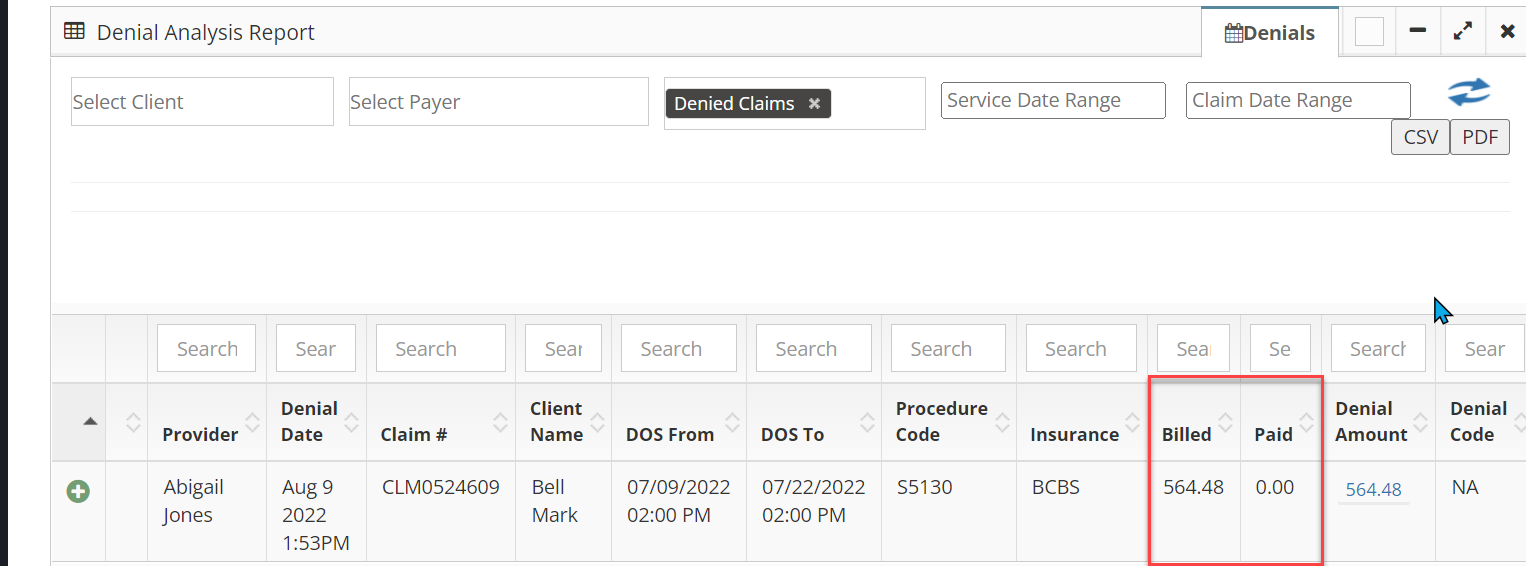
The difference between these amounts, or the money left unaccounted for, is shown by blue text in the Denial Amount column.
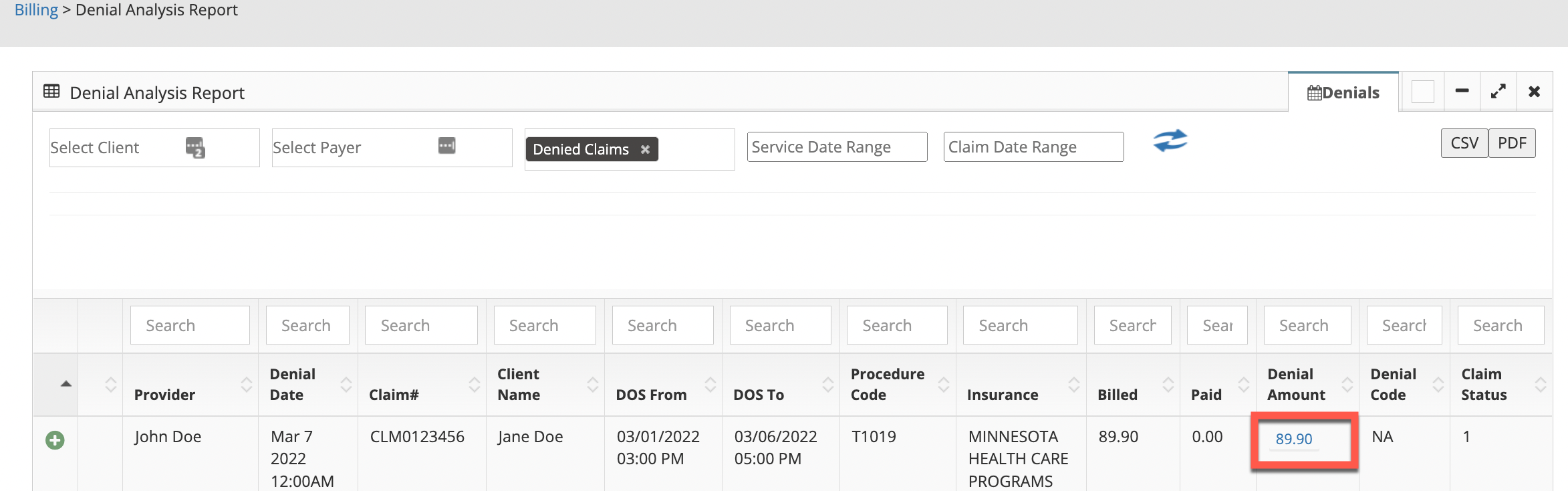
When clicking on Denial Amount the claim can be written off or moved to patient balance so an invoice can be generated to send to the client.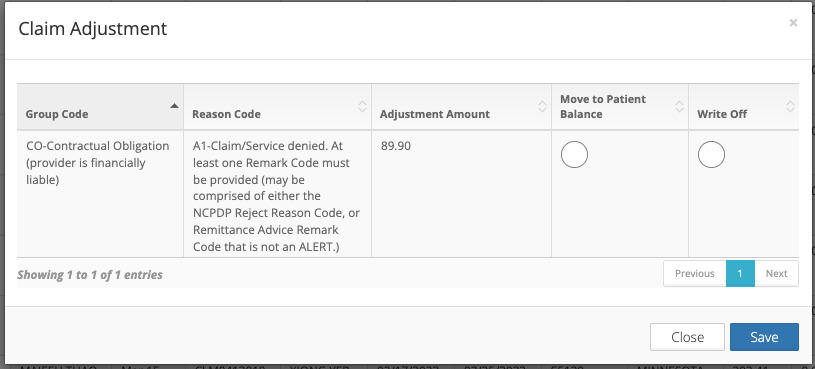
Downloading
To download a CSV or PDF file of the denial analysis report, click on the corresponding buttons in the top right corner.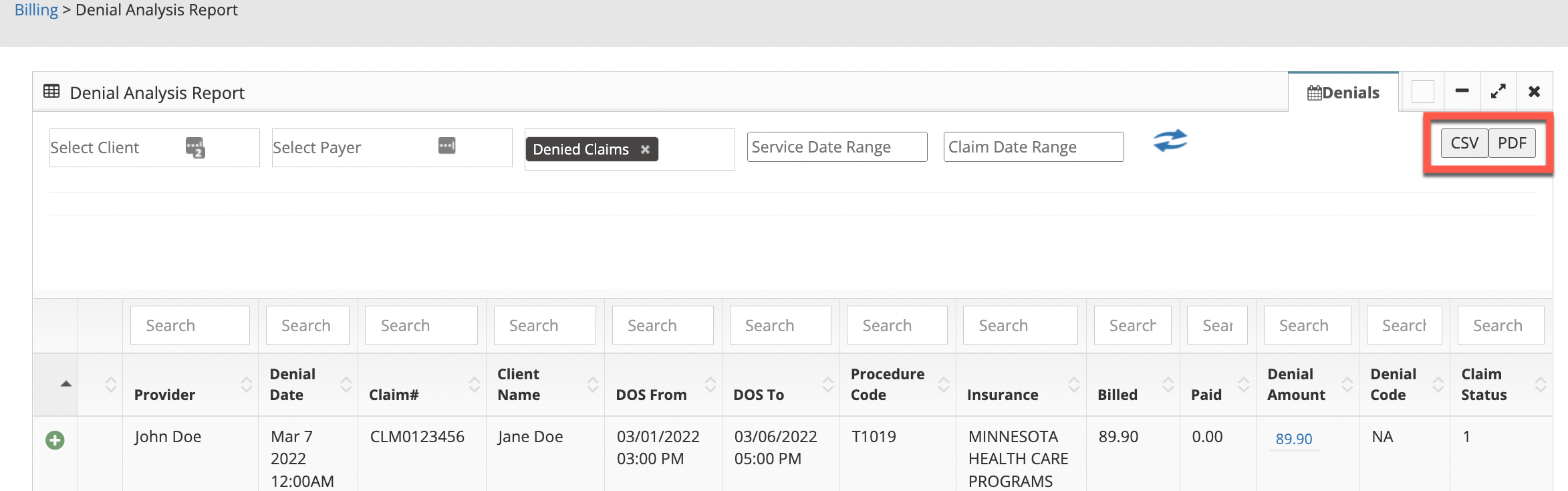
No real client or employee information was used.